Consumer Experience
The multi-factoral analysis that QIDS allows clinicians was critical in helping us to identify where the problem might be, and to then address it
The Quality and Patient Safety Manager at one facility at Sydney Local Health District observed that the rate of hypoglycaemic medication complications per 10,000 bed days was increasing.
The increase coincided with introduction of a new Electronic Medication Management (eMeds) system designed to improve the quality, safety and effectiveness of medication management.
Could it be that eMeds was somehow associated with the rise in complications? A team including health informatics clinicians (nursing, medical and pharmacy) was asked to review.
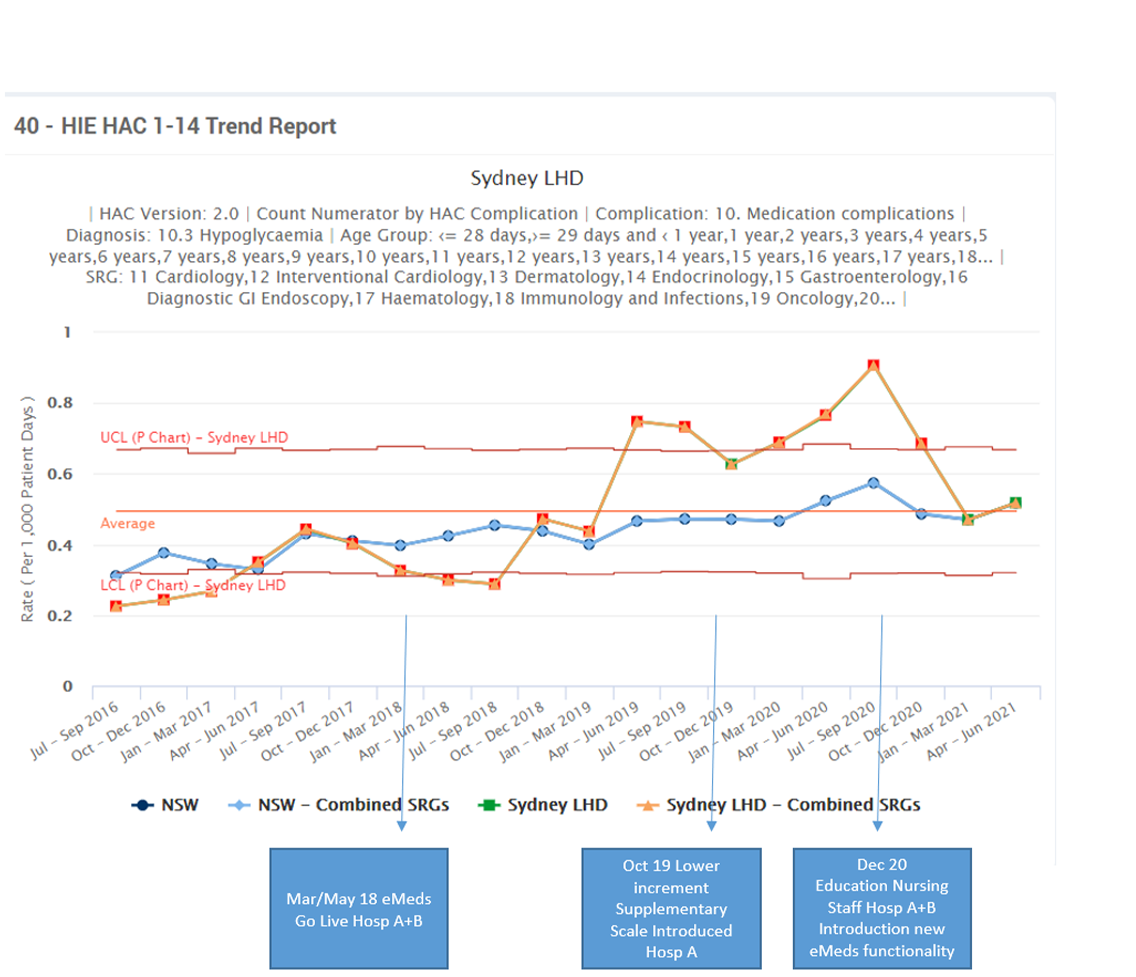
Tracking the reduction in complications from hypoglycaemia using QIDS
The Team
We had two big hospitals – and two very different approaches to insulin. We have built something that will benefit the whole district and allow us to apply a uniform method which will lead to safer outcomes for patients
The team utilised the data analytics tools available through the QIDS, regarding insulin prescribing within the LHD. A systematic review of hypoglycaemic episodes was undertaken analysing the data in a number of ways.
The team identified that they should initially focus on individual patients aged over 75. A comparison of aged care and rehabilitation wards across different hospitals in the LHD showed there was a strong pattern of increases in one hospital.
Within the district there were two ways to prescribe insulin in eMeds – both had advantages and disadvantages. One key difference was the supplemental scales. One had smaller increments then the others. It was thought the scale with smaller increments may be more suitable for elderly patients. This was implemented with some success.
It was time for a deep dive into the QIDS data – picking specific points in time, reviewing cases and enlisting local volunteers to help sift through the data – to help answer the question of whether the build of eMeds could be partially responsible? And, if so, how? This included case reviews.
This analysis showed that eMeds alone was not the answer to the puzzle and that other factors such as nutritional intake could also be involved.
Another line of enquiry was to use eMeds reporting tools to extract the time supplemental insulin was given, which showed a wide variation in patterns.
In order to address the eMeds concerns a working group consisting of endocrinologists, health informatics and eMeds application specialists met to redesign the eMeds build into a Bolus Basal Supplemental PowerPlan. This incorporated improved decision support and assisted nurses in making a cognitive decision during patient treatment.
If this person is not eating should I give insulin?
At the same time, the diabetes team developed and delivered education on diabetes to all nursing staff. Education on the new eMeds configuration was delivered by the Health Informatics team.
Despite the challenges of COVID-19, the changes were implemented at two hospitals on a trial basis with the results carefully monitored utilising eMeds reports and the Glucose Management Mpage (a virtual view allowing clinicians to view all prescribed diabetic medication). The ongoing incidence of hypoglycaemic episodes are monitored through QIDS.
The Hypoglycaemic HAC complication rate is now similar to the NSW rate. It is expected this will further improve once implemented at all hospitals in the District.
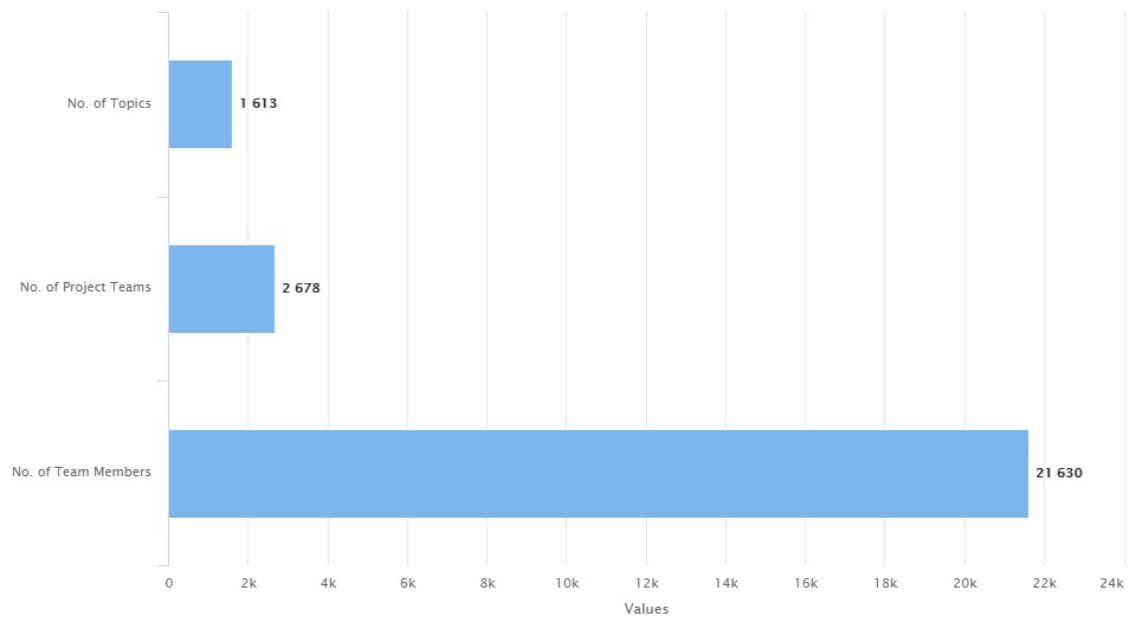
QIDS Improvement projects – more than 20,000 team members are working on QIDS projects
CEC Program
Being able to drill down across a number of facilities was really helpful. Comparison with other settings allows us to better assess performance across the district
The QIDS provides healthcare workers with a single point of access to information and tools to assist in improving the quality and safety of health service delivery.
QIDS transforms data from several sources into a unified platform with standardised and customisable analytic and improvement tools. It enables users to translate raw data into insights such as current outcomes, trends over time, unwanted clinical variation, harm and outcome measures of improvement innovations.
During 2019-2020, QIDS delivered clinical data to more than 29,000 local users in NSW Health, enabling over 800 improvement projects and generating 15,000 monthly reports.
CEC Expertise
We view any case of hypoglycaemic medication complication very seriously – patients can die as a result
QIDS provides a clear picture of clinical factors such as hypoglycaemia at a district level and right down to individual wards.
The improvement quality tool in QIDS allows clinical teams to find issues and raise awareness, and then use QIDS to conduct an improvement project to improve patient outcomes.
