Consumer Experience
A number of ideas were tested to create a smoke-free environment and reduce harm to consumers at Kurrajong, including:
- providing NRT education for staff
- assessing patients’ nicotine dependence and offering NRT
- consistent messaging by staff 'we want to keep you comfortable during your stay with us, please try some NRT'
- coaching a team of nurses to promote a smoke-free environment at morning meetings
- making different types of NRT available
The Kurrajong Smoking Cessation project not only improved the physical health of mental health service consumers through the use of NRT during admission, but reduced aggression and rates of seclusion throughout the trial period.
The Clinical Excellence Commission (CEC) supported the change process through training key personnel as improvement coaches and guiding the team in implementing quality improvement processes.
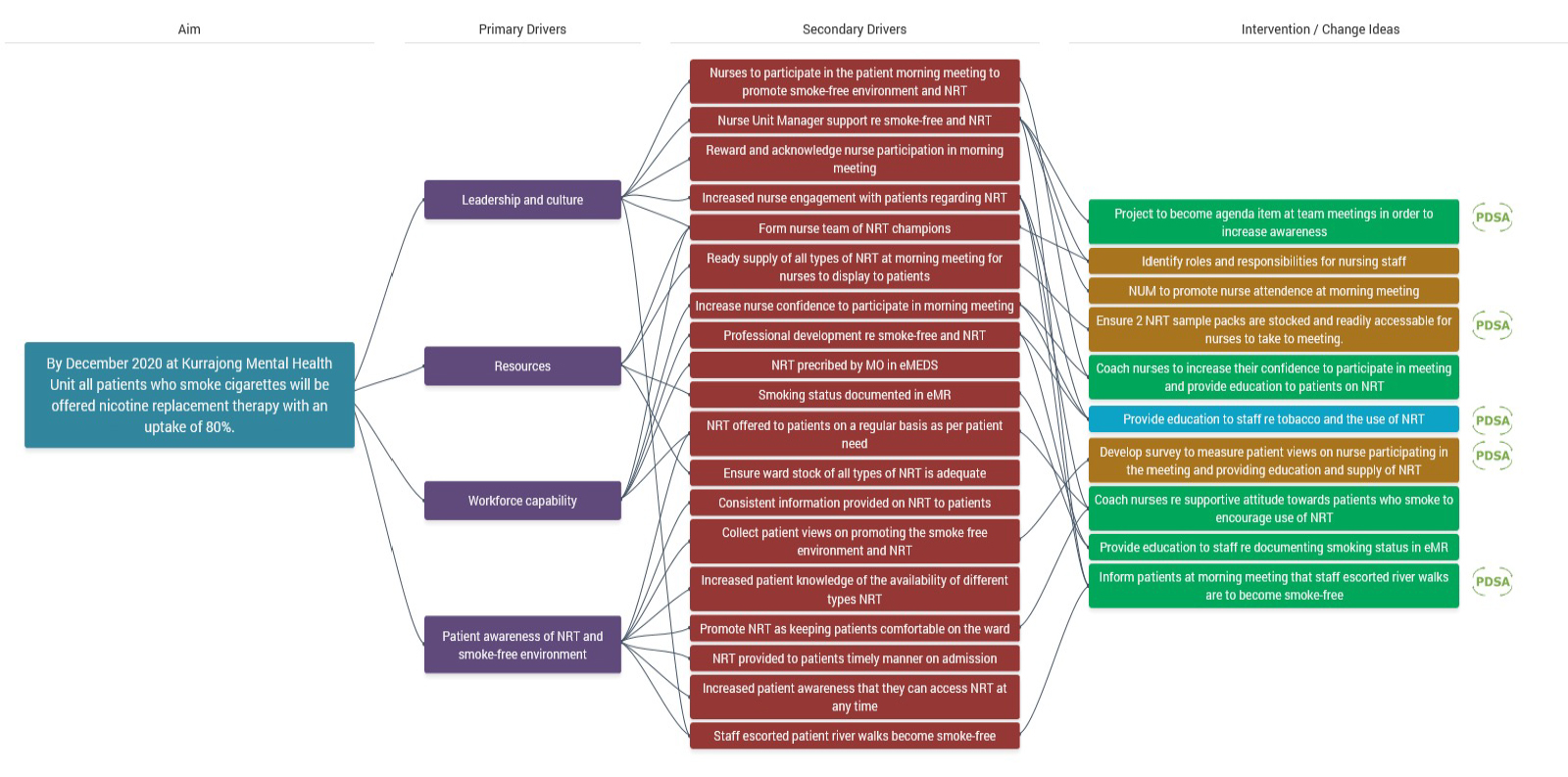
Kurrajong Smoke-free Project Driver Diagram
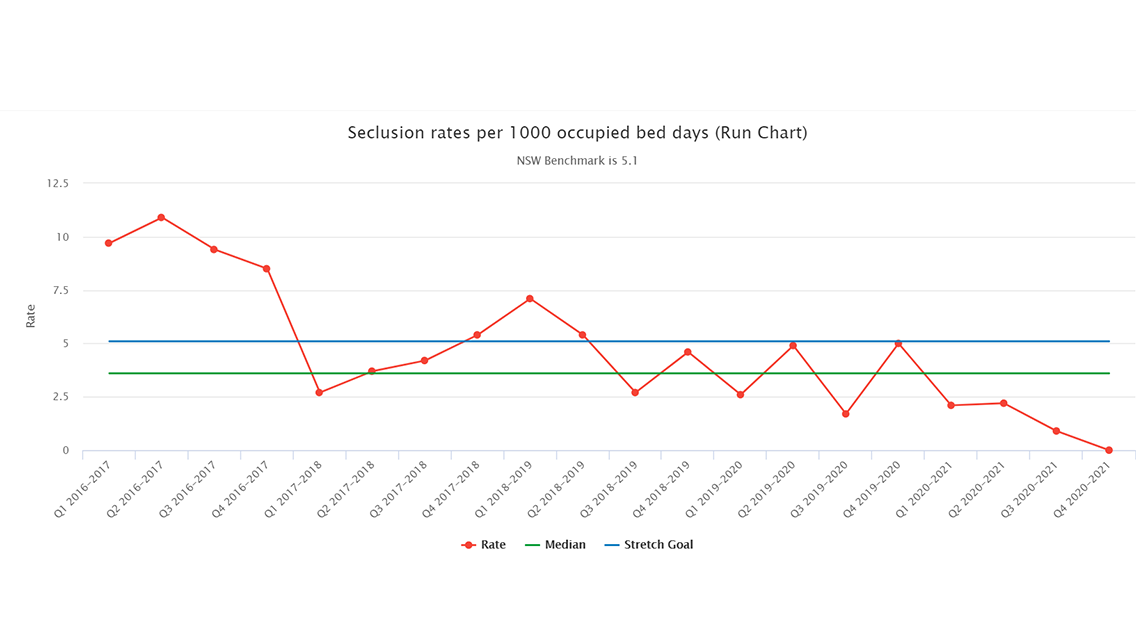
Seclusion Rate per 1000 occupied bed days
In NSW in 2018, 10.8% of the general population smoked cigarettes, in contrast to up to 80% of people with serious mental illness.
This high usage rate has helped to form the belief even among some healthcare workers that patients do not want to quit, or they would find it too much to take on while dealing with treatment, and that they simply wouldn't be able to cope without cigarettes.
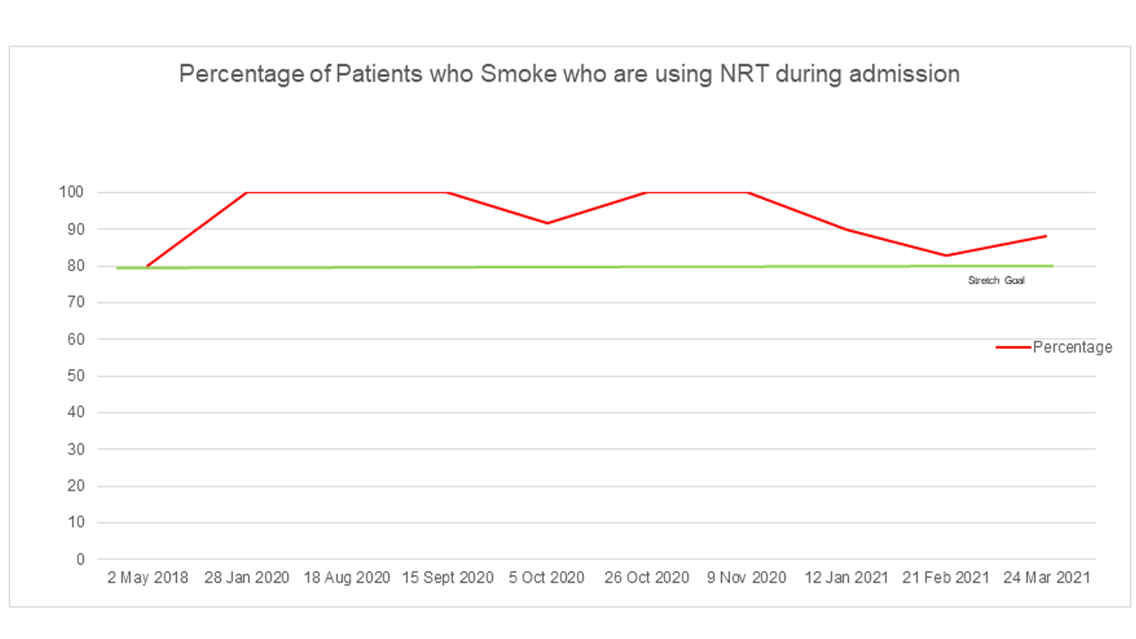
Percentage of patients who used NRT during their admission
Julie Butler, a Mental Health Nurse and improvement coach at Kurrajong said that the success of the “Smoke-free” project in her unit had dispelled those notions and proven that "patients are far more resilient than we give them credit for".
They just need support and a place that is smoke free, if they want to quit, it's up to them. It gives them the confidence that they can actually do it
Lucinda (name changed to protect her privacy) had over 200 admissions to Mental Health Units since her diagnosis, and although she tried cigarettes as a teenager, she started smoking during her first hospital stay because everyone else was smoking, including the staff
From starting to use NRT gum at Kurrajong, and continuing on her return home, Lucinda successfully quit a 40-year tobacco habit within 12 months.
Lucinda has noticed that she does not have a cough anymore and is feeling much healthier, as well as saving a lot of money (she gets a script from the Kurrajong doctors or her GP and gets the NRT gum on the PBS for $6.40 per month). Her goal now is to also wean herself off NRT.
Over an 18-month period, 35 patients at Kurrajong with a variety of diagnoses from schizophrenia to depression have said they are quitting smoking.
To achieve this result amid the COVID-19 pandemic is a significant achievement and provides a quality improvement and patient safety benchmark which the wider mental health system could benefit from.
The Team

Some of the team members of the Kurrajong Smoke-free project. From left: Jennifer Migalic, RN; Julie Butler, CNS2; Lauren Maguire NUM, and Cassandra Porter, CNS1.
The project team at Kurrajong was led by Julie in her capacity as an improvement coach for Northern NSW Mental Health.
Julie received training under the CEC's Mental Health Improvement Coach program, a two-year professional development program which aims to equip Mental Health Improvement Coaches with necessary skills to support mental health teams in their safety and quality improvement work.
The CEC provided Julie and her team with further support and guidance to enable them to conduct testing, demonstrate evidence of the initiative's effectiveness, and help bring their data to life.
The successful collaboration was commended by Mental Health Patient Safety Program (MHPSP) Governance Committee on 25 May 2021.
Thank you again, Julie, for your dedication to testing local ideas to improve consumer and staff safety and wellbeing. It was incredible to see that this has been built into Kurrajong’s way of working and safety culture. Congratulations!
CEC Program
The MHPSP helps the health system create the organisational conditions that enable clinical teams to continually improve the safety and quality of mental health service delivery.
This is being achieved by partnering with consumers and other NSW Health agencies to:
- Explore and understand the current safety and quality improvement landscape in NSW mental health service delivery.
- Co-design a shared vision, agree roles and obtain LHD/SHN commitment to the MHPSP.
- Enhance leadership, capability and culture in safety and quality improvement.
- Establish a state-wide mental health improvement collaborative to support continuous safety and quality improvement and monitoring.
The Mental Health Improvement Coach Program is part of the MHPSP, designed to build LHD/SHN capability in improvement science to reduce harm and improve safety and quality in mental health services across NSW.
CEC Expertise
Between April and August 2019, Julie and 50 others participated in the training that increased their understanding of leadership, coaching and quality improvement to build knowledge and confidence to support their clinical teams to improve safety and quality of mental health care.
The Mental Health Improvement Coach SharePoint site was established to provide a central source of Improvement Coach training resources, recordings of Alumni sessions and other relevant materials.
The Mental Health Improvement Coach QIDS page was created for Improvement Coaches to capture and monitor local improvement initiatives.
I don't go around calling myself an improvement coach, but the Mental Health Improvement Coach Program course has given me the confidence to think I can actually help other people with their quality work
