Consumer Experience
Ray Marshal was admitted to Coledale in December 2019. He spent a total of five months in rehabilitation with two re-admissions to the acute hospital due to complications. Unfortunately, in Ray’s first two months his condition worsened and he was diagnosed with a rare muscular disease that attacks his primary muscle groups. Before admission he had been completely fit and independent, riding motorbikes and making musical instruments.
Ray Marshall, participant in the rehabilitation program at Coledale Hospital
Ray Marshall describes the most difficult point in his illness.
They had to lift me into bed in a sling. To feed myself I had to virtually lay my chin on the table and shovel the food into my mouth because I didn’t want anyone else to feed me. Stubborn I suppose. Yeah I felt really, really bad. I tried to hide it all from my wife. She already had enough on her plate to worry about. But I thought hello I’m bound for a wheelchair here for the rest of my life. I’ll have to have someone to look after me for the rest of my life, and I didn’t feel real good at all really.
I thought Hello. I’m bound for a wheelchair for the rest of my life
When Ray was re-admitted to Coledale Hospital he thought he had lost his independence. As it turns out, the team at Coledale weren’t giving up that easily.
Ray Marshall and Annaliese Getley, Physiotherapist
Annaliese Getley explains the steps in Ray Marshall’s rehab journey
Ok so pretty much for Ray’s journey down the track the hardest thing was for us to make him independent to get out of the chair. First of all he didn’t have enough strength in his shoulders to push himself completely out of the chair but he did have some activation in his legs. So, one of the most pivotal exercises that we were working on was for Ray to just try and push himself out of the chair like so and that probably took us about two weeks to get that done. So, for two weeks Ray worked on that and once he was good enough at that, we then put a frame in front of him. We were pretty confident that if Ray was to walk he’d definitely need a frame and this is the one we decided on. So then we’d then work on coming up, Ray would transition. And to start with he ended up flipping himself back like that because he didn’t have enough tummy control. So from there he had to learn to bring himself forward, and for the first little while, his body would give out and we’d have to help, one or two of us would have to help him get back up. And then we worked on letting go and so Ray managed about 5 or 10 seconds to start with and eventually over the space of about a month we got to a point where he could let go for about a minute for 3 to 5 times. And after he got comfortable with that and doing the full transition, he let us know that he was ready to walk, and so with 2 therapists, a walk belt, Ray took his first few steps down this yellow line and I think he would have walked about 3 to 5 metres to start with.
The Clinical Team

Suzanne Lide signed up for the CEC’s Executive Clinical Leadership Program (ECLP) to expand her skills. This program, aimed at senior clinicians, introduces participants to quality improvement tools such as driver diagramsand run charts. Participants undertake an improvement project which is related to a process or clinical service in which challenges have been identified to put these techniques into action on a real project.
In the ECLP, participants are encouraged to find a problem worth solving. Suzanne identified statistics for patient rehabilitation outcomes at Coledale Hospital were outside the Australasian Rehabilitation Outcome Centres national benchmark data recommendations. Reconditioning following a medical or surgical illness was chosen as the outcome measure as it was noted that the patient length of stay was double the national average for the reconditioning impairment codes. She also found Coledale Hospital patients who presented for reconditioning had a higher Rockwood frailty score and co-morbidities than the national average.
With the problem found, the next step was to find potential solutions in collaboration with the Coledale team.
We completed brainstorming sessions with the whole team and used a quality improvement framework we had used for preventing falls, that is, weekend therapy programs. The idea was that rehabilitation programs could be consumer driven and didn’t need to stop at weekends. When programs continued through weekends, recovery times would improve. Usually program patients would be passively told what to do, we turned that around so patients could continue to work on their recovery over the weekends with the nursing team to guide them.
As part of the ECLP learning program, participants create detailed posters explaining the project, improvement activities and measurement of outcomes.
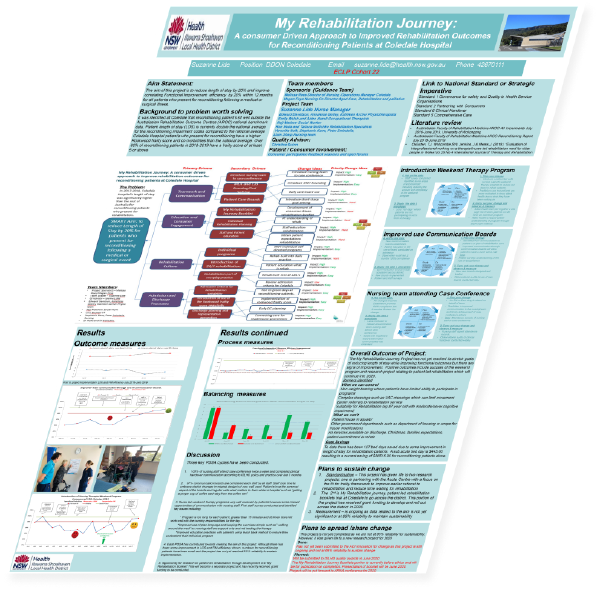
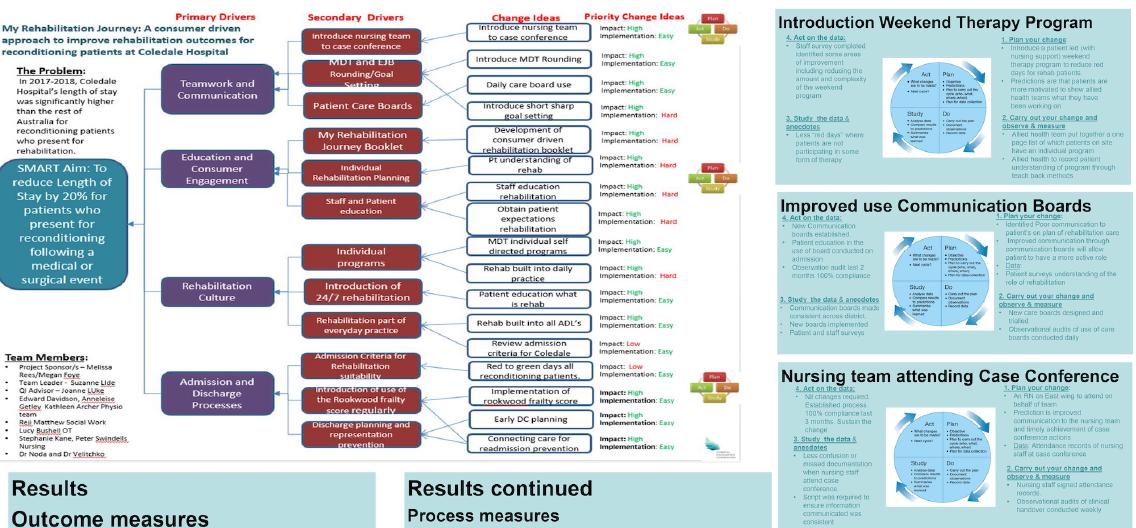
Suzanne Lide’s Project: My Rehabilitation Journey: A consumer Driven Approach to Improved Rehabilitation Outcomes for Reconditioning Patients at Coledale Hospital

Ray’s efforts are celebrated on the Coledale Hospital Success Stories board.

Ray Marshall’s rehab team
Ray attended the gym twice a day every day and was 100% determined to beat the illness. We slowly saw him reverse the effects of his illness, and with the help of his entire team and his supportive family, Ray, at 83 years old walked out of hospital. He regained his independence with activities of daily life which at times still required the use of a wheelchair, however he improved in all of his functional outcomes by greater than 50-80%. He never let his resolve waiver and acted as motivation and support for other patients and staff around him
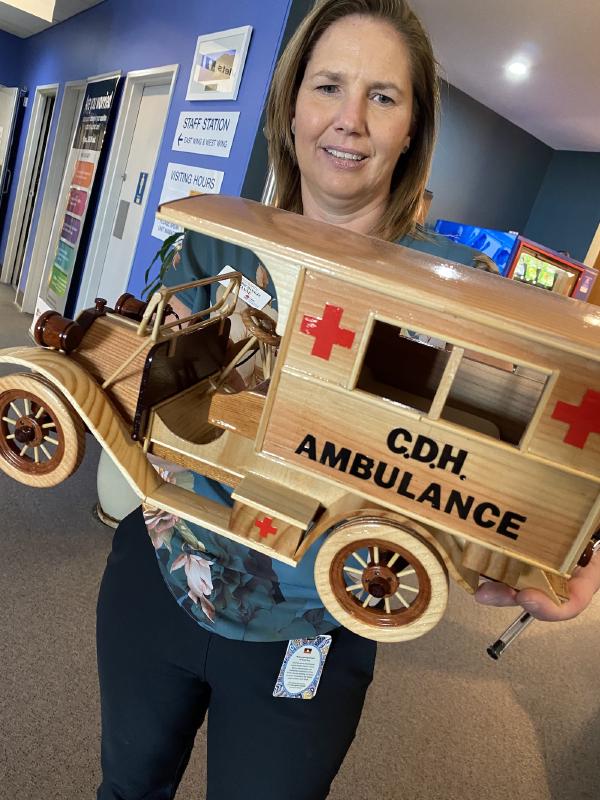
Ray presented the team and the hospital with a hand-made gift.
CEC Program
Suzanne Lide participated in Cohort 22 of the Quality Improvement Academy’s Executive Leadership Program and completed her course as one of 43 participants with a graduation ceremony on 3 March 2020.

Cohort 22 graduation, Suzanne Lide and
CEC Chief Executive, Carrie Marr
The CEC’s Quality Improvement Academy (QIA) is one of the CEC’s key enablers to provide leadership in safety and quality in NSW to improve health care for patients. The QIA aims to support local health districts and specialty health networks to build and sustain the capability needed to support our joint improvement effort. Improvement Science and measurement for improvement is incorporated into the teaching in many of the Academy offerings, including the Executive Clinical Leadership Program and Foundational Clinical Leadership Program.
A central premise of the Academy’s programs is that leadership occurs at all levels in health care and is not dependent on the role of the individual. Leadership learning is based on:
- the process of leading a set of activities that improve the delivery of safe clinical care, and
- the set of attributes required to lead a team, unit, facility, stream or cluster.
Since 2007, the Quality Improvement Academy, has educated over 3,500 leaders across NSW Health as graduates of the Foundational or Executive Clinical Leadership Programs.
In 2019-20, the CEC educated 63 NSW Health staff in the Executive Clinical Leadership Program and 249 graduates in Foundational Clinical Leadership Program through the Quality Improvement Academy, building patient safety and quality capability. Education in improvement science also played a fundamental role in the year’s outcomes for the CEC’s Mental Health Patient Safety Program.
CEC Expertise
Wendy Jamieson holds a Master of Science in Applied Statistics. She has over twenty-five years’ experience in quality management in healthcare with leadership roles in Victoria and NSW. In 2009, she joined the CEC as a member of the Quality Systems Assessment (QSA) team, developing and managing the QSA On-site Visit and Verification Program. In 2015, Wendy was appointed as the Senior Manager of the CEC's Quality Improvement Academy where she managed the Improvement Science and Clinical Leadership Programs with over 400 participant enrolments each year. Wendy is a RABQSA-AU & BSBAUD402B Certified Auditor and successfully completed the ISQuaFellowship Program in June 2014, the CEC Executive Clinical Leadership Program in August 2014 and the USA Institute for Healthcare Improvement Improvement Advisor Program in February 2019.
Wendy Jamieson, Senior Manager, Quality Improvement Academy
Wendy
The feedback has been absolutely fantastic about the programs, they’ve really enjoyed the clinical leadership programs of which we’ve got two - we’ve got the executive clinical leadership program and the foundational clinical leadership program, the feedback has been very positive but also the projects that the staff, the participants have done through these programs has been very beneficial to the patients because they’ve always improved patient care or the safety for patients. It’s important because we want the staff of NSW Health to continually try to improve the care that they give. Improvement science is a great methodology because it teases out the aim of what you are trying to do, it helps you diagnose the actual causes of the problem, using things like driver diagrams and flow charts and also to help come up with ideas to improve patient care but also to measure to see whether the changes that you made an improvement. Highlights for the Quality Improvement Academy over the last year is that despite COVID, we still have been able to deliver our programs and we’ve done this through videoing but also webinars and online using Skype. We’ve also used this time to build a new curriculum which is going to have even more emphasis on patient safety and quality improvement in a contemporary context.
We want the staff of NSW Health to continually try to improve the care that they give.
Ray Marshall walking the yellow lines
Ray Marshall demonstrates his new movement capability.
