Overview
Between the Flags (BTF) provides the foundation for the NSW Deteriorating Patient Safety Net System. It is a 'safety net' for patients built on the principle of early recognition of clinical deterioration based on symptoms and vital sign measurement; standardised systems then ensure any deteriorating patient receives appropriate escalation and care1.
BTF is underpinned by the NSW Health Policy Directive Recognition and management of patients who are deteriorating (PD2020_18) and addresses the Australian Commission on Safety and Quality in Health Care Recognising and Responding to Acute Deterioration Standard.
The BTF system was introduced in NSW in 2010 with the support of the Director-General and has been embedded in 225 acute public health facilities. Implementation was led by the Clinical Excellence Commission (CEC) in collaboration with clinicians, managers, deteriorating patient local leads and a range of other agencies.2
The system is designed to intervene in the process of patient deterioration. The 'Slippery Slope' diagram below illustrates the underlying premise and design concept of the BTF system: early recognition and intervention reduces harm to patients, and the earlier this happens before cardiorespiratory arrest, the better the outcome.
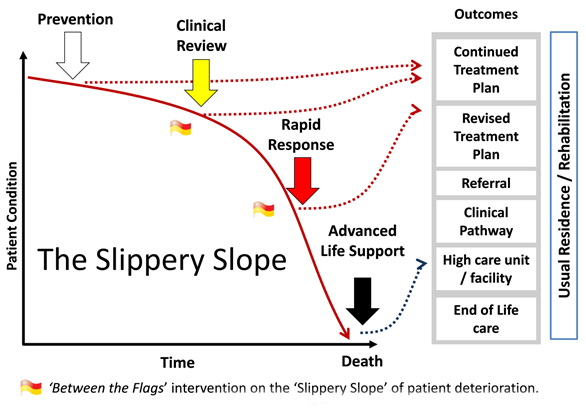
A Clinical Review is a review undertaken within 30 minutes by the clinical team responsible for the patient's care while a Rapid Response is an urgent review by a Rapid Response team (RRT) or locally designated responder/s. Each year more than 84,000 Rapid Response calls alert health workers across NSW to patients who need urgent attention.
The system has widespread staff support and patient care has been made safer and more reliable. The cardiac arrest rate has declined by 42% (P < 0.05) and the Rapid Response rate has increased by 135.9% (P < 0.05).1 Further BTF system outcomes are described in the section on evaluation.
Program elements
The BTF system is designed as a series of interventions that act synergistically. Five inter-dependent elements are needed to deliver improved and sustainable systems for recognition and response to clinical deterioration.
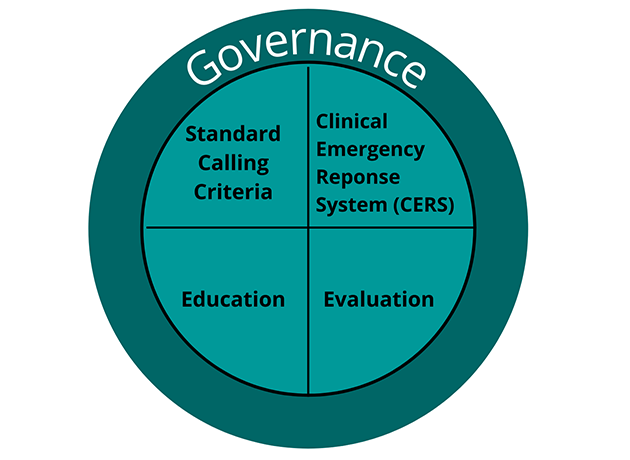
- Governance – structures and processes to support implementation, management and quality improvement at local health district (LHD) and specialty health network (SHN), facility, clinical service and clinical unit level.
- Standard Calling Criteria – including observation charts with standard calling criteria for Clinical Review and Rapid Response and approved local clinical management guidelines/pathways that outline the Clinical Emergency Response System (CERS) response and support documentation.
- Clinical Emergency Response Systems – a local system for the escalation of care that is used by staff, patients, carers and families
- Education – tiered education for clinicians to develop and reinforce clinical and non-technical skills in recognising and responding to patients who are deteriorating.
- Evaluation – an evaluation strategy that includes a family of measures (outcome, process and balancing measures) for monitoring the performance and improving the effectiveness of the Deteriorating Patient Safety Net System.
Links with other programs
BTF provides the foundation for the NSW Deteriorating Patient Safety Net System which is strengthened by the integration of other programs and frameworks, such as:
- SEPSIS KILLS
- End of Life
- Patient, carer and family escalation, known as REACH, and
- Take 2, Think, Do framework for diagnostic error.
The concept of the Slippery Slope has helped LHDs and SHNs to recognise the benefit of safety nets and to develop systems that prevent patients from going down the Slippery Slope in the first place.
Underpinning safe and effective care are high-reliability teams focused on person centered care. Resources and tools are available to help enable safe person centred care through effective partnership, teamwork and communication.
Evaluation
Evaluation of the BTF system is conducted at (1) local level by health facilities and reported to NSW Health and (2) statewide by the CEC to measure the impact of the program and improvements in care of the deteriorating patient.
Health facility evaluation
Local evaluation enables a health facility to know they are providing safe, effective and reliable care for every patient, every time and that the system is working effectively.
The NSW Health Policy Directive Recognition and management of patients who are deteriorating (PD2020_18) requires organisations to have a measurement strategy to monitor the performance and effectiveness of the local Deteriorating Patient Safety Net System.
The measurement strategy should outline a selection of outcome, process and balancing measures. This includes reporting two mandatory quality improvement measures to NSW Health. The measures are:
- Rapid Response call rate per 1,000 acute separations
- Cardio-respiratory arrest rate per 1,000 acute separations.
The CEC Deteriorating Patient Measurement Strategy Guide provides a range of suggested outcome, process and balancing measures to support continuous local improvement in NSW health facilities. Advice on local measurement can be sought from the LHD and SHN deteriorating patient lead and the CEC team.
NSW statewide evaluation
CEC evaluation measures the impact of the program on the statewide health system.
The BTF system model and initial outcomes have been published and recognised internationally. Results show the program has significantly improved the recognition and response for clinically deteriorating patients in NSW public health facilities2. The BTF program is associated with a significant reduction in cardiac arrests in hospitals and ICU admissions secondary to cardiac arrests3.
The CEC has been a national leader in developing a systems approach at scale for recognising and managing deterioration. They have worked collaboratively to share key learnings and resources and a number of Australian states and territories, and international countries have adapted or adopted the standardised observation charts.
References
- Hughes, C, Pain, C, Braithwaite, J et al., 2014, 'Between the flags: implementing a rapid response system at scale', BMJ Quality & Safety, 23(9), 714–717.
- Hughes, C, Pain, C, Braithwaite, J et al., 2017, 'Between the flags: implementing a safety-net system at scale to recognise and manage deteriorating patient in the New South Wales Public Health System', International Journal for Quality in Health Care, 29(1), 130–136
- Ou, L, Chen, J, Hillman, K, et al., 2020, 'The effectiveness of a standardised rapid response system on the reduction of cardiopulmonary arrests and other adverse events among emergency surgical admissions', Resuscitation, 150, 162–169.
- Bhonagiri, D, Lander, H, Green, G, et al., 2020, 'Reduction of in-hospital cardiac arrest rates in intensive care-equipped NSW hospitals in association with implementation of Between the Flags rapid response system', Internal Medicine Journal, 51(3), 375–384.
